News
Study Finds That Common Diabetes Medications Don’t Link to Higher Risk of Autoimmune Rheumatic Diseases
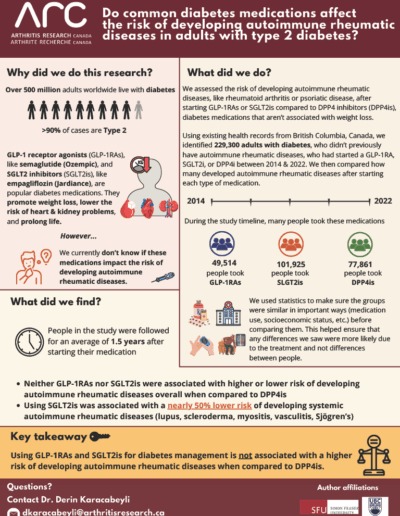
Vancouver (January 8, 2026) – A recent study led by Arthritis Research Canada trainee Dr. Derin Karacabeyli and scientists Dr. J. Antonio Aviña-Zubieta, Dr. Diane Lacaille, and Dr. Hui Xie found that commonly prescribed diabetes medications are not associated with a higher risk of developing autoimmune rheumatic diseases, such as rheumatoid arthritis, psoriasis or psoriatic arthritis, axial spondyloarthritis, lupus, Sjögren’s disease, scleroderma, myositis, and vasculitis.
The study followed 229,300 adults in British Columbia with diabetes who started one of three types of diabetes medications between 2014 and 2022 and hadn’t been diagnosed with an autoimmune rheumatic disease before. Participants were followed for an average of about one and a half years after beginning treatment.
The team wanted to assess the risk of developing autoimmune rheumatic diseases after starting GLP-1 RAs receptor agonists or SGLT2 inhibitors compared to DPP4 inhibitors. GLP-1 medicines, which are glucagon-like peptide-1 receptor agonists like semaglutide (Ozempic), and SGLT2 inhibitors, which are sodium glucose co-transporter 2 inhibitors like empagliflozin (Jardiance), promote weight loss. Medications like DPP4 inhibitors, which are dipeptidyl peptidase-4 inhibitors like sitagliptin (Januvia), do not promote weight loss. Prior studies showed that DPP4 inhibitors do not increase the risk of developing autoimmune rheumatic diseases, so people taking these medications served as a control group.
After accounting for differences between people starting each type of medication, the team found that neither GLP-1 medicines nor SGLT2 inhibitors were linked with higher or lower risk of developing autoimmune rheumatic diseases, compared to DPP4 inhibitors, except for one subtype, systemic autoimmune rheumatic diseases, which include lupus, Sjögren’s disease, scleroderma, myositis, and vasculitis. People using SGLT2 inhibitors had a 50 per cent lower risk of developing this type of diseases compared to people using DPP4 inhibitors.
“GLP-1 medications and SGLT2 inhibitors are being used more and more, so it’s important that we continue exploring their effects on the immune system,” said Karacabeyli.
“We found no safety concern with the use of these medications – people were not more likely to develop auto-immune rheumatic diseases. Additionally, our results suggest that using SGLT2 inhibitors might reduce the risk of developing systemic autoimmune rheumatic diseases. More research is needed to test whether this finding is reproducible in different settings, and to better understand how this effect occurs.”
Read the full study here.
-30-
Infographic
Click to enlarge document.
ABOUT ARTHRITIS RESEARCH CANADA:
Arthritis Research Canada is the largest clinical arthritis research institution in North America. Our mission is to transform the lives of people impacted by arthritis through patient-centred research and engagement. Arthritis Research Canada is home to a team of over 100 researchers, trainees and staff whose life-changing research is creating a future where people with arthritis have the knowledge and tools to triumph over pain and disability. Arthritis Research Canada is conducting research from coast to coast with centres in British Columbia, Alberta, Ontario, Quebec, and Nova Scotia and scientists affiliated with 10 major Canadian universities.
For more information or to arrange an interview, please contact:
Bernice Rahman
Marketing and Communications Officer
Arthritis Research Canada
brahman@arthritisresearch.ca