The Arthritis Newsletter
Winter 2015Cardiovascular Disease Risk for People Living with Inflammatory Arthritis
If you have inflammatory arthritis, you should be aware of the increased risk of developing cardiovascular disease (CVD), and the increased risk of dying early from heart and blood vessel problems. In fact, people with inflammatory arthritis are at risk of dying up to a decade earlier from CVD than the general population. Researchers are studying ways of preventing early death for those affected with inflammatory arthritis. Inflammatory arthritis includes rheumatoid arthritis (RA), lupus and related diseases (psoriatic arthritis, gout, and ankylosing spondylitis).
There are ways to reduce your risk with proper risk assessment screening, lifestyle changes and treatment of underlying causes. Read Dr. Claire Barber’s interview, watch the recommended videos, and read Soheila’s story to discover:
1. How inflammatory arthritis causes heart attacks, strokes and blood clots (video link below)
2. Who is at risk for heart disease and why (video link below)
3. What real-life consequences can occur when a patient’s caregivers do not link CVD risk and inflammatory arthritis. Soheila, (link to her story below) experienced two mini-strokes and one major stroke. Her story illustrates a sobering gap in CVD risk and cares for those with inflammatory arthritis.
4. How Dr. Claire Barber’s leading-edge research (interview transcript follows) is addressing these gaps in care. Dr. Barber is developing a timely system to help health care practitioners identify and monitor CVD risk for RA patients. The outcomes of this research could highly influence a patient’s care and could possibly be applied to other inflammatory disease groups. Claire’s work is an important FIRST STEP in this field on a national and international level and was recently recognized by her rheumatology colleagues with the initial publication of her research.
Arthritis Patient Advisory Board (APAB) members sat down with Claire to discuss her research…
Claire, what inspired you to do work in this field?
As a practicing rheumatologist, I have a real interest and passion for improving the quality of care for patients. I identified a massive gap in this area of the cardiac risk for arthritis patients and I am passionate about closing this gap between patients, primary care providers (general practitioners) and rheumatologists.
Compared to the general population, patients with RA have about a 50% higher mortality rate if they have a cardiovascular event. In addition, RA patients with well-established CVD risk factors such as hypertension are not identified and managed consistently.
I hope to reduce CVD risk in RA patients by better identifying and managing risk factors that CAN be modified such as smoking, hypertension, obesity and high lipid levels.
In commenting on my research, the Journal of Rheumatology states “There is evidence pointing to variation in practice and to deficiencies in
recognition and treatment of traditional CV factors in patients with RA. Then the ultimate goal of developing RA specific guidelines for CVD primary prevention would be to facilitate a broader understanding of best practices and provide metrics for rheumatology care providers to ensure they are delivering high-value care toward primary prevention of CVD in patients with RA.”
What did you and your team accomplish, and how will this research be used?
We developed a set of quality indicators that capture the essence of high-quality care so that doctors and health care systems can define areas and targets for improvement.
To develop the 11 quality indicators, I first conducted a systematic review of best practices for CVD preventive care. I then formed an in-person international expert panel to develop a potential “candidate” list of quality indicators and then convened an online international panel and utilized an innovative software platform.
The result?
A practical process list to be provided to rheumatologists, cardiologists and primary care providers that can be used to help educate and train [them] to realize efficient, reliable and high-quality CVD preventive care to people with RA.
This list of 11 key processes also specifies what is to be measured, in whom, and in what period of time.
Focusing on the process rather than outcome measures means the clinical practice will be improved and CVD prevention should be enhanced. As an example, combining a specific screening procedure (e.g. blood pressure over 140/90) with a specific clinical action (e.g. advising the primary care provider of the need for treatment or additional follow up).
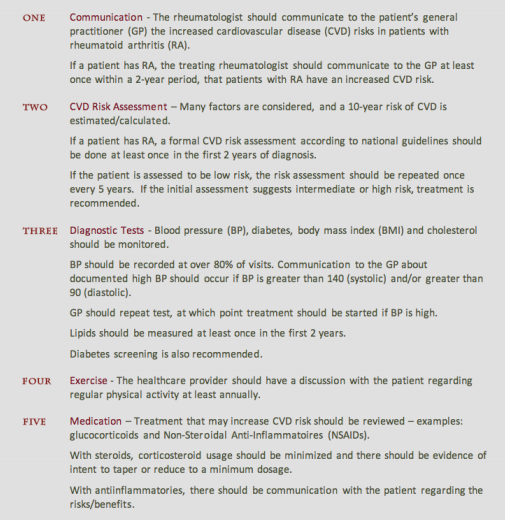
Key processes grouped into five themes:
What are the main messages in your research?
First, our patients who have a substantially higher risk need to be proactive with screening (e.g. exercise, diabetes, and medications can have an impact). Therefore, early screening and rescreening at regular intervals is critical!
Secondly, if you don’t measure it, you can’t change it! For RA patients’ quality of care to improve in Canada, you need to be able to document and measure it, and this is simply not possible in many areas of the country. You can’t make a difference until you show the numbers, so this is a plea for a mandate to drive change. Government and third parties need to drive improvement in quality metrics for the benefit of our patients.
There is currently a huge gap in the health care system, and there is a need to move quality indicators (for best standards of practice) FORWARD!
What other professional groups will be able to benefit from your research?
The research will hopefully be helpful in educating many different groups ultimately with the goal of helping monitor comorbidities [the presence of one or more additional disorders or diseases cooccurring with a primary disease or disorder].
Potentially there is a huge role of also educating and coordinating with allied health professionals, pharmacists, and physiotherapists, for example.
This work is soon to be presented to family practice practitioners in Alberta.
What is the next phase of your research?
My thesis ended with development and testing, so the next step is implementation. I have tested this “list” with my clinic in Alberta and results are currently submitted for publication. The next issue is implementation and patient input is sought to determine who should be involved in monitoring.
Further applications?
This process of developing “best practices” could be applied to other disease groups and is easily modified for other inflammatory diseases (e.g. lupus, SARDS, etc). Lupus patients in particular face even higher cardiac risk due to lupus blood factors and potential renal involvement (kidneys).
Thank you, Claire! We are grateful that you have dedicated your career to improving the quality of care for patients. These are exciting times with many more opportunities to engage in and benefit from your research!
As patients, we can help ARC researcher Dr. Claire Barber move her research to action. Talk to your GP and rheumatologist about cardiovascular risk and arthritis – share these recommendations and this article!
Video Resources & Soheila’s Story (links coming soon):
Dr. Antonio Avina, MD, MSc, PhD, FRCPC – How arthritis causes heart attacks, strokes and blood clots.
Dr. Diane Lacaille, MDCM, MHSc, FRCPC – Who is at risk at heart disease and why.
Journal reference:
C.E. Barber, D.A. Marshall, N. Alvarez, et al. Development of Cardiovascular Quality Indicators for RA: Results from an International Expert Panel Using a Novel Online Process.
The Journal Of Rheumatology
J.M. Davis III. Toward Quality of Cardiovascular Preventive Care for Patients with Rheumatic Diseases Editorial




















































